Let’s talk about health care issues in Canada. Canada has long boasted one of the most accomplished health care systems in the world. Universal, publicly funded and accessible, Canadians have demonstrated that their health care system ranks among the top globally in terms of equity and outcomes for the general population.
Even the most innovative and forward-thinking health programs face significant challenges. Canada is no exception. What are the persistent health care issues in Canada, particularly affecting Indigenous populations, that the country continues to address with renewed urgency and comprehensive policy reforms?
Indigenous health care disparities in Canada
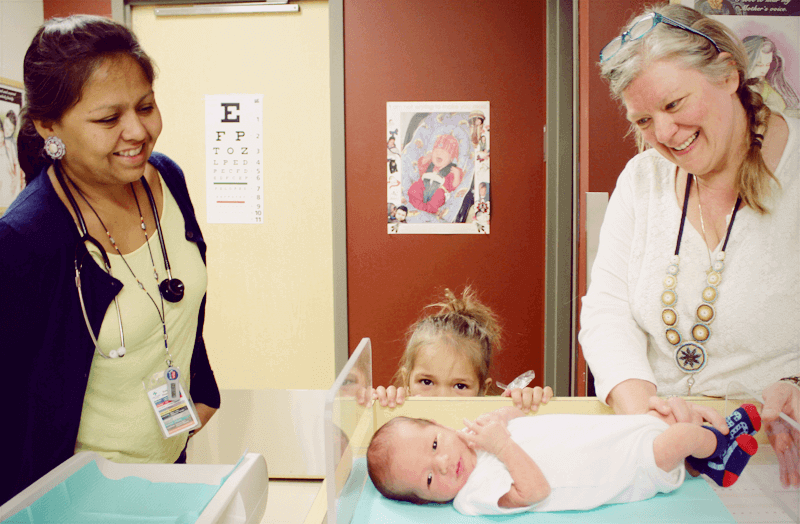
While Canada has focused on providing universal health care coverage, significant gaps persist in serving Indigenous communities. First Nations, Métis, and Inuit populations face complex health challenges rooted in geographic isolation, historical trauma, and systemic barriers that continue to impact health outcomes today.
“The health disparities faced by Indigenous peoples in Canada are not just statistics – they represent a fundamental challenge to our commitment to equity in healthcare,” explains Dr. Janet Smylie, a leading Indigenous health researcher at St. Michael’s Hospital. “Geographic barriers are just one layer of a complex web of issues that require comprehensive, culturally appropriate solutions.”
Key health disparities and access barriers
The scope of Indigenous health challenges extends far beyond simple geographic access. Current data reveals stark disparities across multiple health indicators:
- Life expectancy gap: Indigenous populations have a life expectancy 5-15 years lower than the Canadian average
- Chronic disease rates: Higher incidence of diabetes (3-5 times the national rate), cardiovascular disease, and respiratory conditions
- Mental health crisis: Suicide rates among First Nations youth are 5-7 times the national average
- Maternal and child health: Infant mortality rates remain significantly higher in Indigenous communities
- Infectious disease burden: Higher rates of tuberculosis and other preventable diseases
Access challenges and systemic barriers
Multiple factors contribute to ongoing health disparities in Indigenous communities:
Geographic and Infrastructure Barriers:
- Over 100 First Nations communities lack year-round road access
- Medical transportation costs can exceed $10,000 per emergency evacuation
- Limited high-speed internet affects telemedicine capabilities
- Ongoing water advisories in dozens of communities impact basic health and sanitation
Healthcare System Gaps:
- Shortage of healthcare providers willing to work in remote locations
- Complex jurisdictional issues between federal, provincial, and territorial governments
- Cultural competency gaps among non-Indigenous healthcare providers
- Limited integration of traditional healing practices with western medicine
Current government initiatives and progress
Recent federal investments and policy changes demonstrate renewed commitment to addressing these disparities. The 2023-2025 period has seen significant developments:
Recent Policy Developments:
- $6 billion investment (2023-2028): Dedicated funding for Indigenous health transformation
- Jordan’s Principle expansion: Ensuring First Nations children receive necessary health, social, and educational services
- Indigenous Health Equity Fund: $2.5 billion specifically for mental health and addiction services
- Community-based care models: Supporting Indigenous-led health governance and service delivery
National Chief RoseAnne Archibald of the Assembly of First Nations noted in 2024: “We’re seeing unprecedented federal investment, but the real measure of success will be whether these funds translate into measurable health improvements in our communities. Self-determination in healthcare delivery is essential for sustainable progress.”
Indigenous health must remain a national priority
Canada has made substantial progress in recognizing the historical impacts of colonization on Indigenous health outcomes. The Truth and Reconciliation Commission’s Calls to Action have provided a roadmap for addressing systemic inequities through concrete policy changes and increased funding commitments.
However, meaningful change requires sustained commitment beyond political cycles. Indigenous communities have demonstrated remarkable resilience and are increasingly taking leadership roles in designing and implementing culturally appropriate health solutions that blend traditional knowledge with modern medical practices.
Measuring progress and accountability
To ensure meaningful progress, Canada has established specific targets and accountability measures:
2030 Health Equity Targets:
- Reduce the life expectancy gap by 50% by 2030
- Eliminate all long-term drinking water advisories by 2026
- Increase Indigenous healthcare provider representation to 4% of the national workforce
- Establish comprehensive mental health services in 600+ Indigenous communities
- Achieve 90% childhood immunization rates in all Indigenous communities
The path forward
Following its universal healthcare principles, Canada must continue prioritizing Indigenous health equity through sustained investment and policy reform. The federal government’s approach now emphasizes Indigenous self-determination in healthcare delivery, recognizing that communities are best positioned to identify their own health priorities and solutions.
Essential water infrastructure, mental health services, and culturally competent care remain immediate priorities that require ongoing attention and resources. The integration of traditional healing practices with western medicine, supported by adequate funding and policy frameworks, represents a promising path toward more holistic and effective healthcare delivery.
Canada’s commitment to closing health gaps for Indigenous populations reflects the country’s broader values of equity and social justice. With proper implementation of current initiatives and continued community engagement, the next decade could see transformative improvements in Indigenous health outcomes, serving as a model for other nations facing similar challenges.

